The NIH’s set of studies around long covid are called RECOVER (I assume it’s an acronym because it’s always in all caps? Edited 12/17 to add: found it in a The People’s CDC newsletter! “The Researching COVID to Enhance Recovery (RECOVER) initiative”). I’ve heard many concerns around the studies they’re doing, but they’re also the biggest funding source so I signed up hoping that at least some of the studies would be beneficial. The first step is to do a phone interview and some questionnaires to identify what symptoms I have. The official list for long covid has over 200 symptoms and everyone has a different subset. Once they have established a profile you can start enrolling in the specific studies.
A researcher in Boston is doing a study on sleep (aptly named RECOVER-SLEEP) with two different cohorts. One is for insomnia and the other is for hypersomnia.
The questionnaire to sort me into the sub-study asked about how much sleep I get, if it’s refreshing, and if I’m tired during the day. One of my concerns is there’s no differentiation between fatigue and feeling tired in the surveys. I’m always fatigued. I never feel refreshed upon waking. And I’m also not able to fall asleep during the day. I will occasionally struggle to fall asleep at night – especially after a day where I exerted beyond my capacity – but this isn’t a major symptom for me. I generally fall asleep easily, stay asleep a long time (at least 9 hours), wake up feeling fatigued, and force myself to rest throughout the day. I say force myself to rest because most days I’m capable in the moment of doing lots more than I can do without consequences. I get post exertional malaise (PEM) if I use more physical, mental, and emotional energy than my body can produce. This is the defining characteristic of myalgic encephalomyelitis (ME). So if I don’t force rest throughout the day I have more symptoms and increased severity of my baseline symptoms for the next few days. I honestly would rather be more tired if I have to have ME because it would make pacing easier.
Based on the questionnaire I was placed in the Hypersomnia sub-study. This makes sense since I’m sleeping more than the average person and still feeling fatigued.
I decided to enroll in this study since fatigue is one of my top 3 most debilitating symptoms and I was hoping the trial was for a treatment for long covid that would alleviate some of my fatigue. More specifically, I had assumed that the medication they were studying was trying to treat an underlying cause or condition that people with long covid have. After telling me I qualify for the hypersomnia study the research assistant described the medication as a stimulant. This set off red flags because I’m very sensitive to stimulants, and because if people who don’t understand ME feel more awake without resolving the actual disease that’s going to lead to a crash (small amounts of over-exertion result in PEM, continuing to push through PEM results in serious consequences like a decrease in baseline function and long term symptom flares).
I expressed my concerns right away to the research assistant. They didn’t know any more than the script in front of them so they arranged for me to speak to the lead researcher who is a doctor (the lead at the Mass General site, not at the NIH). While I was waiting for that conversation I was also able to review the consent form. It says “The study drug will be either modafinil (Provigil) or a placebo pill. Modafinil (pronounced mow-DAH-fuh-nil) is a pill taken by mouth and is used to help people to stay awake during the day.” As a reminder, I don’t need help staying awake. I’m awake all day, I have low energy while awake. The researcher said the drug exits your system quickly so if I have issues because I’m sensitive to stimulants I could stop taking it immediately and it would be cleared from my system in 12 hours. He also said that no one understands long covid chronic fatigue or post exertional fatigue and so the goal of this study is to see if this drug affects them.
In the moment that all sounded reasonable and so I signed the consent and we did the blood draw. I have a Garmin that helps me with pacing and I thought “I can withdraw immediately if things go the way I think they will.” But then during the car ride home I felt less sure.
- I don’t like that he called it post exertional fatigue – I get lots more symptoms than fatigue if I overdo it. PEM is often described as “flu like symptoms” – it’s a whole set of symptoms including fatigue, muscle aches, congestion, sore throat etc. And my list of symptoms increases every few months. This spring I added an acidic feeling in my stomach to my PEM list, this fall I added pruned fingers (bodies are weird). I had flushing in my ears and face a few hours after I got home from the research visit from the exertion of driving and answering lots of questions (cognitive exertion requires a lot of energy).
- While it’s true that long covid is new and we don’t have a lot of clarity on long covid chronic fatigue, it’s simply false to say we have no understanding to build from. Post viral illnesses are not new. ME is not new. Both have been significantly underfunded (see also: conditions that impact a much higher proportion of women than men) but they have been researched.
- I’m not confident I won’t have a longer recovery time from any adverse reaction to the study drug. Most people may metabolize the drug quickly but my system is very fragile. I tried topomax for headaches over the summer and the raspy voice I developed as a side effect lasted months past when I stopped taking it.
- If I’m on the placebo then I have to do 15 weeks of work for something I don’t think we should be spending energy studying.
All of that to say: I dropped out of the study after having more time to think. This decision was further validated when I asked my long covid discussion group about this study and someone found a research study on the drug they’re testing. I didn’t read the full study but right there in the abstract it says “The use of wakefulness-promoting agents is discouraged for addressing unexplained fatigue, as seen in the context of chronic fatigue syndrome.” (ME was originally called chronic fatigue syndrome before more research was done to understand that the mechanisms are related to muscle, brain, and inflammation – myalgic encephalomyelitis is those words in Latin/medical. The name chronic fatigue syndrome is still common among people who do not understand the extent of the condition.)
How did no one read that study before designing this clinical trial? At the very least there should be clearly stated risk factors. The risk factors in this consent form talk about how you might feel frustration while completing cognitive tasks and you might get a bruise from a blood draw. There’s nothing about the significant risk of increased symptoms if people believe themselves to be better and push beyond their actual capacity. I’m very concerned people who don’t realize they have PEM will be harmed by this study. I’m also concerned that the only people who stay in the study for a full 15 weeks will be people who have a type of long covid that doesn’t include PEM. If that happens, and there was no screening for PEM as part of enrollment, this study could be published as evidence this drug cures long covid fatigue. That is the most dangerous outcome as then doctors around the world could push this medication plus exercise on people who won’t know until they’re severely disabled that pushing through until burnout can be disastrous for people with ME.
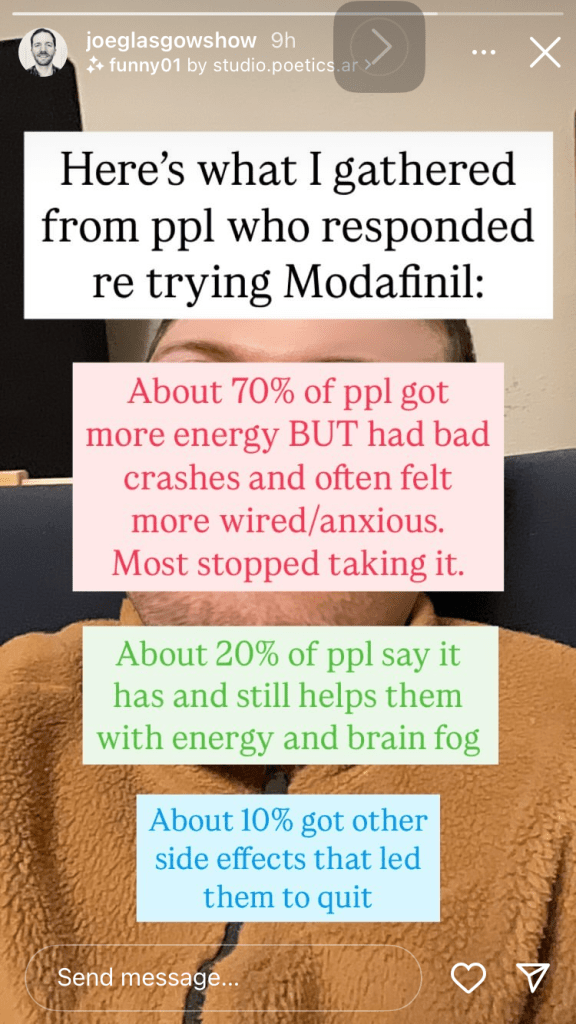
This concern is entirely based in reality. It’s already happening, as you can see from an informal survey done by someone with long covid on Instagram. A study backed by the NIH is only going to make this misinformation about how to deal with fatigue caused by long covid/ME more widespread.
Additional thought after I hit post the first time: The other cohort that has insomnia rather than hypersomnia seems less dangerous. They’re getting melatonin and light box therapy. They are still in the same boat of addressing a symptom without consideration of the underlying cause.
Email to the IRB:
All of the above plus: A member of my long covid discussion group reached out to their contact at the NIH after I posted, the contact said “The study co-chairs have been discussing this scenario and what education the sites need including clarity and language around the specific sleep phenotypes that RECOVER SLEEP is studying. The Project Leader is going to keep me updated on key discussion points and how the re-education of sites and support for participants is being carried out. I (and the study co-chairs) are thankful that this person reached out to you, and that you shared the email with me.” It is very concerning to me that the project leads have identified issues with the study and are continuing to recruit for it with complete disregard to the consequences.
Email to the local research team:
All of the above plus:
In addition to my concerns about the study at large, there are also things you can be doing to better support participants at your particular site. Everyone you are inviting to join the study has issues with sleep which automatically results in a level of cognitive impairment, and many folks with long covid have additional brain fog on top of that. Reducing cognitive load is essential for limiting the exertion required to participate.
- Explain the parking and public transit options before people arrive (I did not know that the address you gave me landed me at valet parking.)
- Explain the financial aspects (Do you validate parking? Reimburse for parking?)
- Explain exactly how to reach the office (Do I check in at the front desk? Which elevator do I use?)
- Estimate how long each appointment will be (I need to rest in advance and plan recovery time)
- Ask about access needs (Participants may use a wheelchair to reduce exertion. I need text either read aloud or sent to my phone)
Doing any one of these things can help reduce the strain of participation. My symptoms increased after the appointment and it’s taken over a week for me to be able to write all of this, partially because of the PEM I faced after the appointment.
